Arrhytmias and device treatment
Arrhythmias encompass brady-arrhythmia and tachyarrhythmia. Brady-arrhythmia effectively treated by pacemaker implantation is growing. Specialized pacemakers stimulating both ventricles (Cardiac Resynchronization Therapy – CRT) have proved effective for selected heart failure patients. Effective treatment of tachyarrhythmia has been developed. Radiofrequency ablation is curative for many patients and a promising technology also for a growing number of patients with atrial fibrillation and ventricular tachycardia. Implantable cardioverter defibrillator (ICD) therapy is effective for primary and secondary prevention of sudden cardiac death.
Cardiac pacing
The optimal mode of cardiac pacing is important for patient outcome. Our team has studied pacing mode selection for decades (Andersen et al. 1997, Nielsen et al. 2011), and also new and potentially improved pacing options (Albertsen et al. 2008, Kronborg et al. 2011)With improving technologies and techniques, larger focus is on optimizing device treatment and avoiding complications (Johansen et al. 2011, Kirkfeldt et al. 2011).
Cardiac Resynchronization Therapy
For patients with heart failure and prolonged ventricular activation cardiac resynchronization therapy (CRT) reduces morbidity and mortality (Kronborg et al. 2008). We study the improvement and optimization of CRT; patient selection, left ventricular lead placement (Kronborg et al. 2009) and device programming.
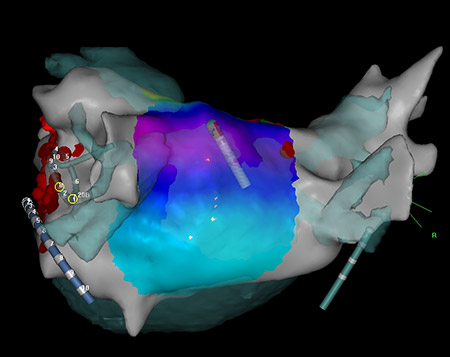
Scar related tachycardia
Atrial tachycardia is a significant problem after cardiac surgery involving atrial incisions. We have considerable experience in ablation of these in congenital heart disease, after mitral valve surgery and heart transplantation. We have performedsingle-center (Lukac et al. 2005), as well as multicenter studies (Lukac et al. 2009) in this area. We disclosed the arrhythmogenic propensity of the transseptal approach to mitral valve surgery (Lukac et al. 2006). Continuation of this work is ongoing to preventscar-related tachycardias (Lukac et al. 2007) .
Cardiac Autonomic Nervous System
The function of the cardiac autonomic nervous system can be estimated by various non-invasive electrocardiographic techniques. The activity in the parasympathetic and sympathetic nervous system plays an important role in the pathophysiology of sudden cardiac death, is significantly altered in diabetic patients where it may play a role for blood pressure regulation and other complications. In malignant vasovagal syncope changes in cardiac autonomic balance plays a salutary role in the final pathways of the hemodynamic collaps. However, many of the cause-effect relations are unclarified.
The ECG laboratorium and syncope clinic offers various ECG technics for the estimation of cardiac autonomic activity primarily based on heart rate variability and investigations of hemodynamic changes in relation to orthostatic stress.
The technics have been used in the evaluation of the mechanism of atrial fibrillation post CABG; in the role of the autonomic neuropathy in diabetic patients for blood pressure control and other complications; the impact of vagal activity on the cardiac repolarization process; factors of importance for prolonged depolarization – Late Potentials, and the effects of drugs on the cardiac autonomic balance.
There is also an interdisciplinary research cooperation with neurological departments on the role of myocardial ischemia, myocardial fibrosis – late potentials and autonomic abnormalities for the patophysiology of unexplained death in epilepsy, and studies on the changes in and the role of autonomic imbalance in chronic pain disorders. The technics are also used in the studies of early cardiac changes in neurodegenerative diseases in children.
The findings in studies of the patophysiology of vasovagal syncope, have founded an ongoing international clinical study on closed loop pacing in patients with neurocardiogenic syncope.
Contacts
Rikke Esberg Kirkfeldt, MD, PhD-student, kirkfeldt@dadlnet.dk
Anders Sommer Knudsen, MD, PhD-student, a.knudsen@dadlnet.dk
Mads Brix Kronborg, MD, PhD., mads.brix.kronborg@ki.au.dk
Christian Gerdes, MD, PhD., consultant in cardiology and electrophysiology, chr.gerdes@dadlnet.dk
Henrik Kjærulf Jensen, MD, DMSci, PhD, associate professor, consultant in cardiology and electrophysiology, hkjensen@ki.au.dk
Peter Lukac, MD, PhD., consultant in cardiology and electrophysiology, lukac@ki.au.dk
Peter Mortensen, MD, consultant in cardiology and electrophysiology, PTM@KI.AU.DK
Jens Cosedis Nielsen, MD, DMSci, OhD., associate professor, jenniels@rm.dk
Henning Mølgaard, M.D., DMSci., Associate Professor, Consultant ; E-mail: h.molgaard@dadlnet.dk
Current co-workers:
Astrid Juhl Terkelsen, M.D., PhD., senior registrar, Department of Neurology; E-mail: astrid@akhphd.au.dk
John Østergaard, M.D., DMSci, Professor,Department of Paediatrics, Centre for Rare Diseases.E-mail: johnoestergaard@skejby.rm.dk