Accelerated Diagnosis and Decision Support in acute stroke
Our two research groups develop tools to help physicians during time-critical decision-making and treatment. After an acute ischemic stroke, it is estimated that 1-2 million neurons die every minute until blood flow is restored. The therapies in question, however, must not be administered to patients with hemorrhagic stroke, and carry some risk of adverse events in ischemic stroke patients, especially late after symptom onset. We therefore develop artificial intelligence (AI) systems that (i) instantly provide physicians with prognostic information based on each patient’s MR images and clinical findings and (ii) help physicians discover new, safe, and efficient therapies. Also, we seek to detect biological markers that can help diagnose hemorrhagic and ischemic stroke during transport to the hospital, which would make it possible to start pre-hospital treatment in the future.
Predicting stroke outcome in individual patients – and the efficacy of therapies
Several image modalities are often combined when assessing acute stroke patients: Diffusion weighted images to detect ischemic tissue injury, susceptibility weighted imaging to detect hemorrhages, and perfusion weighted imaging to detect hypoperfused tissue that might be salvaged by immediate restoration of blood flow. We took part in the development and validation of these modalities in acute stroke, and now develop ways to assess the relative benefits of various treatment options in individual stroke patients.
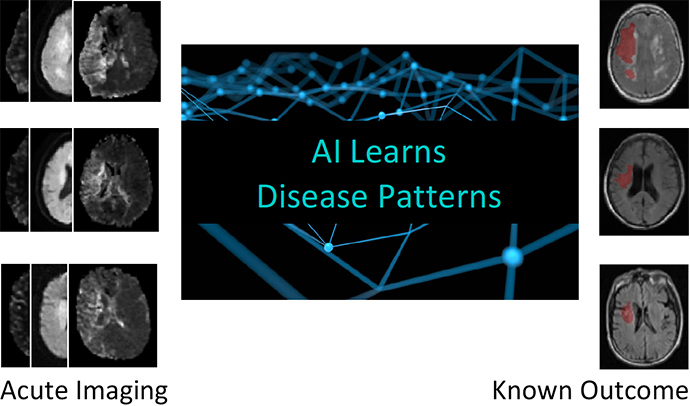
To do this, we use artificial intelligence (AI) algorithms to trace the fate of brain tissue from hundreds of previous patients, each with different co-morbidities, symptom duration, hundreds of affected image voxels with different levels of diffusion, perfusion, and CTH changes (See Capillary Dysfunction group webpage); patients are offered different treatments. By comparing this information to their follow-up images, showing which image voxels survived the ischemia, the algorithms can estimate the risk of infarction across hypoperfused tissue in new patients, providing radiologists and neurologists with immediate access to prior experience from similar patients at other hospitals. This information, in the form of maps, shows patients’ risk of losing specific tissue regions because of the stroke and the different available treatment options.
This approach is also an efficient way to assess benefits of new therapies – in terms of the extent to which they reduce the risk of infarction for tissue subjected to various degrees of hypoperfusion and capillary dysfunction. By comparing these risks between treated and untreated patients, any risk-reducing effects can be detected with a high degree of certainty in small patient cohorts – and be used to inform whether larger randomized trials should be conducted.
Pre-hospital diagnosis – and therapy?
To allow earlier diagnosis and treatment of stroke patients, we also develop new diagnostic devices that evaluate multiple biomarkers simultaneously in blood samples acquired by ambulance staff. As no single biomarker has been found able to stratify stroke patients so far, we hypothesize that the simultaneous evaluation of multiple biomarkers could allow us to reach this goal. In particular, we want to test if biomarkers on small nano-sized extracellular vesicles (EVs) can be used for early stroke diagnosis. Secreted EVs readily cross the blood-brain-barrier (BBB) and we speculate that EV content and surface properties change rapidly – reflecting the state of the secreting cells within the brain.
We hope this approach will enable the development of a diagnostic device that can categorize patients according to their stroke type. To this end, we will use AI algorithms to link EV data with clinical data and neuroimaging findings from existing patients, where the diagnosis and stroke type is known. We hope this approach will identify biomarkers distinctive for the different stroke types. This will be the first step towards a portable diagnostic device to be used in a prehospital setting, enabling certain treatments to be initiated in the ambulance.
References
- Nielsen A, Hansen MB, Tietze A, Mouridsen K. Prediction of Tissue Outcome and Assessment of Treatment Effect in Acute Ischemic Stroke Using Deep Learning. Stroke. 2018; 49(6):1394-1401. doi: 10.1161/STROKEAHA.117.019740.
- Livne M, Boldsen JK, Mikkelsen IK, Fiebach JB, Sobesky J, Mouridsen K. Boosted Tree Model Reforms Multimodal Magnetic Resonance Imaging Infarct Prediction in Acute Stroke. Stroke. 2018;49(4):912-918. doi: 10.1161/STROKEAHA.117.019440.
- Boldsen JK, Engedal TS, Pedraza S, Cho TH, Thomalla G, Nighoghossian N, Baron JC, Fiehler J, Østergaard L, Mouridsen K. Better Diffusion Segmentation in Acute Ischemic Stroke Through Automatic Tree Learning Anomaly Segmentation. Front Neuroinform. 2018; 12:21. doi: 10.3389/fninf.2018.00021.
- Blauenfeldt RA, Hougaard KD, Mouridsen K, Andersen G High Prestroke Physical Activity Is Associated with Reduced Infarct Growth in Acute Ischemic Stroke Patients Treated with Intravenous tPA and Randomized to Remote Ischemic Perconditioning. Cerebrovascular Diseases 2017; 44: 88-95. doi: 10.1159/000477359
- Just J, Yan Y, Farup J, Sieljacks P, Sloth M, Venø M, Gu T, de Paoli FV, Nyengaard JR, Bæk R, Jørgensen MM, Kjems J, Vissing K, Drasbek KR. Blood flow-restricted resistance exercise alters the surface profile, miRNA cargo and functional impact of circulating extracellular vesicles. Sci Rep. 2020;10(1):5835. doi: 10.1038/s41598-020-62456-3.
- Stenz KT, Just J, Blauenfeldt RA, Drasbek KR. Extracellular Vesicles in Acute Stroke Diagnostics. Biomedicines 2020; 28;8(8):248. doi: 10.3390/biomedicines8080248.
Contacts
Professor Kim Beuchau Mouridsen, email: kim@cfin.au.dk
Associate Professor Kim Ryun Drasbek, email: ryun@cfin.au.dk