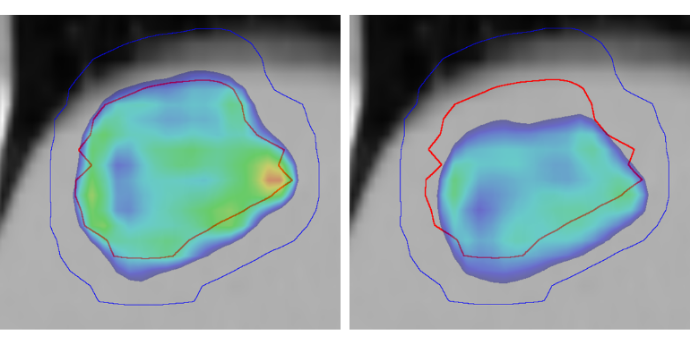
 Planned (left) and delivered (right) dose to a liver tumor (red contour) as calculated in real time during a treatment fraction with substantial tumor drift. Only high doses above 95% are shown (adapted from Skouboe et al. Radiother Oncol 2019: 139, 66-71).
Planned (left) and delivered (right) dose to a liver tumor (red contour) as calculated in real time during a treatment fraction with substantial tumor drift. Only high doses above 95% are shown (adapted from Skouboe et al. Radiother Oncol 2019: 139, 66-71).
In radiotherapy, ionizing radiation is used to kill cancer cells, but the treatment will unavoidably also damage normal tissue. It is therefore important to maximize the effect of radiotherapy on tumor cells and minimize the effect in normal tissue. Our research group work on two strategies to achieve this.
The first strategy is to physically hit the tumor more precisely with the radiation beams while dose to normal tissue is minimized. A great challenge is that tumors and normal tissue often move during radiotherapy delivery, e.g. due to respiration, heartbeat and rectum or bladder filling. The motion can lead to a dose distribution that differs substantially from the planned dose (see the image above). We develop methods for real-time tumor motion monitoring during treatment delivery, real-time treatment adaptation to the motion, and real-time calculation of the dose as it is being delivered to the moving anatomy. Such methods can ensure that suboptimal dose delivery caused by motion is detected and hindered. On a longer time scale, knowledge of the actual dose delivered to the patient, rather than just the planned dose, will improve our understanding of dose-response relationships in radiotherapy.
FLASH is the other strategy that we are investigating to maximize tumor damages relative to normal tissue damages. FLASH is radiotherapy delivered with ultra-high dose rates that are more than 100 times faster than in conventional radiotherapy. FLASH has received massive attention since animal experiments have shown remarkable sparing of normal tissue when compared to conventional dose, while the effect on tumors is unaltered. The mechanism behind the differential effect of FLASH on tumor and healthy tissue is not yet understood, and the exact conditions to trigger the FLASH effect remain to be determined.
We investigate different aspects of FLASH delivered with proton pencil beam scanning and electron beams such as FLASH beam generation and characterization, FLASH compatible dose measurements, the FLASH effect in radiobiology studies, FLASH effect modelling, FLASH treatment planning and motion management methods.
People
 Professor of medical physics
Professor of medical physics
Per Rugaard Poulsen
per.poulsen@rm.dk
Further information.
 PhD student
PhD student
Sky Rohrer
JANROH@rm.dk
 PhD student
PhD student
Karolina Alexandra Klucznik
karolina.klucznik@rm.dk
PhD student
Valentin Vacari Møller
valentin.m@rm.dk
 Visiting PhD student
Visiting PhD student
Sara Shahzadeh
SASHAH@rm.dk
Collaborating researchers
 Associate professor of medical physics
Associate professor of medical physics
Jacob Graversen Johansen
jacjoa@rm.dk
Further information.
 Novo Nordisk Foundation Professor of experimental particle therapy and radiobiology
Novo Nordisk Foundation Professor of experimental particle therapy and radiobiology
Brita Singers Sørensen
bsin@oncology.au.dk
Further information.
 Professor of medical physics
Professor of medical physics
Ludvig Muren
ludvmure@rm.dk
Further information.
Medical Physicist, PhD, Dep. of Oncology, MedFys
Thomas Ravkilde
PURE, Aarhus University. Further information.
Medical Physicist, PhD, Dep. Of Oncology
Esben Worm
esbeworm@rm.dk
Associate professor
Jesper Folsted Kallehauge
jespkall@rm.dk.
Further information.
 Associate professor of medical physics
Associate professor of medical physics
Lone Hoffman
Lone.Hoffmann@aarhus.rm.dk
 Associate professor of medical physics
Associate professor of medical physics
Ditte Sloth Møller
dittmoel@rm.dk.
PURE, Aarhus University.
Medical Physicist, PhD
Anne Vestergaard
annveste@rm.dk
Medical Physicist
Jakob Borup Thomsen
JAKTHS@rm.dk
Medical Physicist
Jørgen Breede Baltzer Petersen
joerpete@rm.dk.
PURE, Aarhus University. Further information.
Medical Physicist
Liliana Stolarczyk
LILSTO@rm.dk