Lung and oesophageal cancers are some of the most frequent cancers worldwide. Patients are treated with chemo-radiotherapy with curative intent. However, for both cancers, a high risk of local relapses and distant metastasis results in low overall survival rates five years after diagnosis.
The research group at the Department of Oncology at Aarhus University Hospital/The Danish Centre for Particle Therapy consists of medical physicists and oncologists. We focus on finding the optimal radiotherapy strategy for lung and oesophageal cancer patients through research projects and clinical trials. The work includes:
- Adaptive radiotherapy
Anatomical changes occurring during the radiotherapy course lasting five to six weeks may result in dose deterioration for the target and over-dosage of radiosensitive normal tissue. We are world-leading in adaptive radiotherapy and implemented adaptive radiotherapy for lung cancer patients in 2013, which led to a significant increase in overall survival concurrently with a dramatic reduction in side effects. - Modelling
Based on imaging, dosimetric, clinical and follow-up data for both lung and oesophageal cancer patients, we do modelling studies on TCP and NTPC in order to pave the way for patient-individualised radiotherapy. - National clinical trials
In collaboration with DOLG (Danish Oncological Lung Cancer Group), we run several national and international clinical trials on e.g. dose escalation, hypo-fractionation, and palliation. All protocols require high clinical and technical standards. - European multi-centre clinical trial PROTECT
Randomised proton versus photon trial with very high-quality assurance. The protocol emerges from Aarhus University Hospital and we are chairs for the international project quality assurance group. - Robustness of proton planning
Proton therapy is highly sensitive to anatomical changes and respiratory motion. By optimising the planning and treatment delivery, the robustness of proton therapy can be increased. For oesophageal cancer, we have shown that proper selection of beam angles leads to proton plans being more robust than photon plans. We run randomised trials for both lung and oesophageal cancer patients.
- AI for organs at risk definition
AI may secure more standardised and uniform delineation for organs at risk. We have implemented AI for the delineation of all organs at risk in the thoracic region based on delineations made during a national workshop for experienced oncologists. Similarly, AI will be used for the delineation of organs at risk in other anatomical regions - Autoplaning
Clinical dose plans may depend heavily on the dose planner and are furthermore resource-demanding. Automation in dose planning may result in more standardised plans and potentially reduce the dose to the organs at risk. We are working on implementing automation in dose planning. - eFLASH
FLASH reduces toxicity to organs at risk while maintaining the same dose to the tumour. FLASH may be delivered using conventional electron beams transferred into FLASH mode. We work on the dosimetry related to clinical use of eFLASH
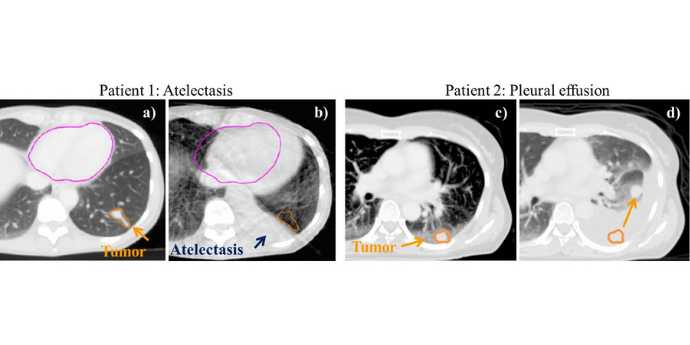 RT is planned on a CT. Each day, a cone-beam CT is acquired before treatment. For patient 1 and 2, tumors are clearly visible on the plan CTs (a) and (c), while the appearance of atelectasis in patient 1 (b), and pleural effusion in patient 2 (d) are observed on the cone-beam CTs. For both patients, the tumor is pushed away from the original position and the tumor dose is lower than planned if the treatment is not adapted to the new anatomy.
RT is planned on a CT. Each day, a cone-beam CT is acquired before treatment. For patient 1 and 2, tumors are clearly visible on the plan CTs (a) and (c), while the appearance of atelectasis in patient 1 (b), and pleural effusion in patient 2 (d) are observed on the cone-beam CTs. For both patients, the tumor is pushed away from the original position and the tumor dose is lower than planned if the treatment is not adapted to the new anatomy.
People
 Head of Medical Physics, AUH Oncology Dept.
Head of Medical Physics, AUH Oncology Dept.
Ditte Sloth Møller
dittmoel@rm.dk
Further information.
 Associate professor of medical physics
Associate professor of medical physics
Lone Hoffmann
lone.hoffmann@aarhus.rm.dk
Further information.
PhD student
Simon Nyberg Thomsen
SIOTOM@rm.dk
PhD student
Sarah Eckholdt Jensen
SAECJE@rm.dk
Senior registrar
Hanna Rahbek Mortensen
Hanna.Mortensen@auh.rm.dk
Medical Physicist
Mai Lykkegaard Ehmsen
mai.ehmsen@rm.dk
Medical Physicist
Maria Fuglsang Jensen
marfugje@rm.dk
Consultant, Dep. of Oncology, Aarhus University Hospital
Marianne Marquard Knap
mari.knap@auh.rm.dk
Consultant, associate professor, Dep. of Oncology, Aarhus University Hospital
Azza Khalil
azza.khalil@auh.rm.dk
Consultant, associate professor, Dep. of Oncology, Aarhus University Hospital
Marianne Nordsmark
marianne.nordsmark@rm.dk
Medical physicist, Dep. of Oncology, Aarhus University Hospital
Christina Maria Lutz
chrilutz@rm.dk